2020 Research Grants
The AMRF has awarded the 2020 research projects. Quality applications were received from around the country to make a very competitive field.
Thanks to our generous donors throughout the year, we are once again thrilled to announce our research grants for 2020.
In line with our vision going forward, these grants continue the work in different areas of research which investigate the many different pathways that will ultimately change outcomes for people diagnosed with melanoma, and to improve the current alarming statistics.
It is only with the support of our melanoma community, AMRF team and board that we can strive to achieve the best outcome now and for future generations.
We wish to acknowledge the incredible support given by donors, volunteers and fundraisers Australia wide. Thank you.
Early Career Researcher
Identification of prognostic melanoma autoantibodies
Dr Pauline Zaenker
Edith Cowan University, Perth
Postgraduate
Research into liver metastases from cutaneous (skin) melanoma
PhD student Jordan Conway
Uni Sydney, MIA
Postgraduate
Research into early detection of uveal (eye) melanoma
PhD student Aaron Beasley
Edith Cowan University, Perth
Identification of prognostic melanoma autoantibodies
Dr Pauline Zaenker
Edith Cowan University, Perth
Dr Pauline Zaenker, a postdoctoral research fellow at Edith Cowan University (ECU) in Perth has been awarded one of the 2020 Australian Melanoma Research Foundation (AMRF) Early Career Scientist Grants. Dr Zaenker is a long-standing member of the Melanoma Research Group at ECU who are experts in the identification of blood-based biomarkers in patients with melanoma and other malignancies.
Dr Zaenker specialises in the identification of cancer-associated autoantibodies, markers of the patients’ immune response, for the diagnosis of melanoma from a simple blood sample. In this project and with the help from the AMRF, Dr Zaenker will work alongside Associate Professor Elin Gray, leader of the Melanoma Research Group (ECU), and Masters by Research student Miss Desiree Sexauer to follow up a large cohort of early stage melanoma patients and test whether autoantibody levels at the time of diagnosis of the primary melanoma tumour could serve as an indicator of risk of the melanoma to spread and an indicator of shortened overall patient survival.
The research team anticipate that the knowledge gained from this study will contribute towards the future development of a simple blood test in the clinic that may be used as an additional tool to further strengthen the ongoing surveillance of melanoma.
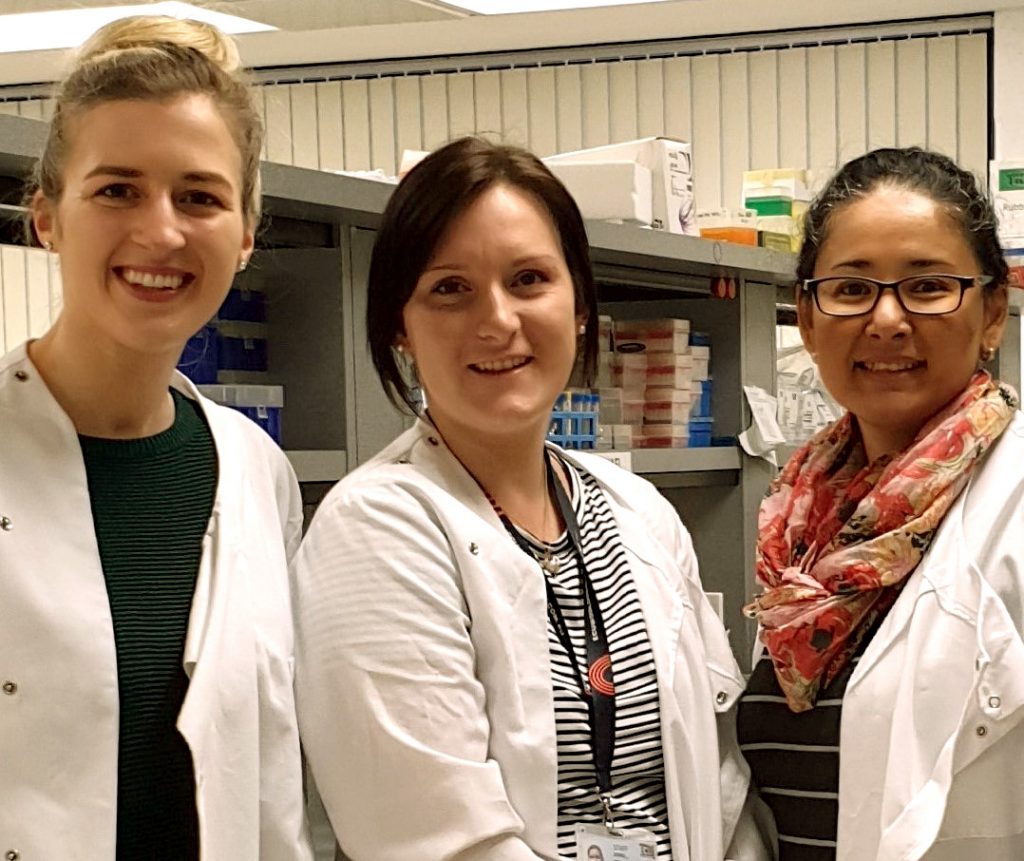
Miss Desiree Sexauer, Dr Pauline Zaenker and Associate Professor Elin Gray
June 2022 update
Dr Pauline Zaenker has the following update to share with us.
Project description and summary
Cutaneous melanoma is the most aggressive type of skin cancer that is responsible for more than 80% of skin cancer-related deaths. The incidence of cutaneous melanoma, especially thin (< 1.0 mm) melanomas, continues to increase nationally and globally. Although thick (≥ 4.0 mm) melanomas are correlated with a worse prognosis, thin melanomas account for the majority of melanoma deaths due to the high volume of the disease. Therefore, there is currently an urgent need to identify melanoma-associated prognostic biomarkers for the effective monitoring of patients that are predicted to have an increased risk of tumour progression. This will enable timely therapeutic intervention and ultimately decrease melanoma attributed morbidity and mortality.
The utilisation of autoantibodies as melanoma-associated biomarkers is a promising avenue towards personalised medicine. Autoantibodies are generated by the adaptive immune system in cancer patients towards autologous antigens and may provide biological information of the tumour. Additionally, autoantibodies have desirable biomarker properties such as persistent concentrations and long half-lives due to a limited proteolysis and clearance from the blood.
The overarching aim of this project was to identify serum autoantibody biomarkers from blood that are indicative of disease progression. Early-stage cutaneous melanoma patients provided a blood sample at the point of diagnosis of their primary melanoma. Follow-up data (average of 3.83 years) of melanoma progression and patient survival was then received from the Western Australian Clinical Cancer Registry.
A total of 104 sera were previously screened against a functional high-throughput microarray platform containing 1627 functional proteins to measure IgG autoantibody levels. The Clinical Cancer Registry data has been used to group the early-stage cutaneous melanoma cohort into a progression versus non-progression group. The prognostic utility of tumour protein 53 (p53) autoantibody as a prognostic biomarker was extensively examined due to literature suggesting its high potential as a prognostic biomarker. The microarray and bead-based immunoassay results indicated that p53 autoantibodies were found not to be of significant prognostic value as a single prognostic marker in this melanoma cohort. Its prognostic value as part of a larger autoantibody panel remains to be validated.
Furthermore, superoxide dismutase 1 (SOD1) autoantibodies were identified as a potential marker for melanoma progression. The subsequent investigation of SOD1 antibodies via a bead-based immunoassay has shown that SOD1 autoantibodies might be of significant value for the prognostication of early-stage cutaneous melanoma patients. There was, however, a degree of discordance identified between the two platforms. Additionally, the Melanoma Institute of Australia newly developed Nomogram tool that predicts the sentinel lymph node (SLN) metastasis risk for early-stage cutaneous melanoma patients has been used to investigate whether autoantibodies measured at the point of diagnosis might be valuable in predicting whether a melanoma patient has an increased risk of developing SLN metastasis. The prognostic value of tumour-necrosis factor alpha-induced protein 8 (TNFAIP8) has been investigated following its identification as a potential top prognostic marker based on the microarray data. The subsequent bead-based immunoassay to validate the finding has shown that TNFAIP8 autoantibodies as a single biomarker has limited value in discriminating predicted high-risk from predicted low-risk patients. There was a weak correlation and a poor level of agreement identified between the two platforms.
This work was presented at the Australian Society of Medical Research conference 2020, the Australian Melanoma Conference 2021 and the World Melanoma Conference 2021.

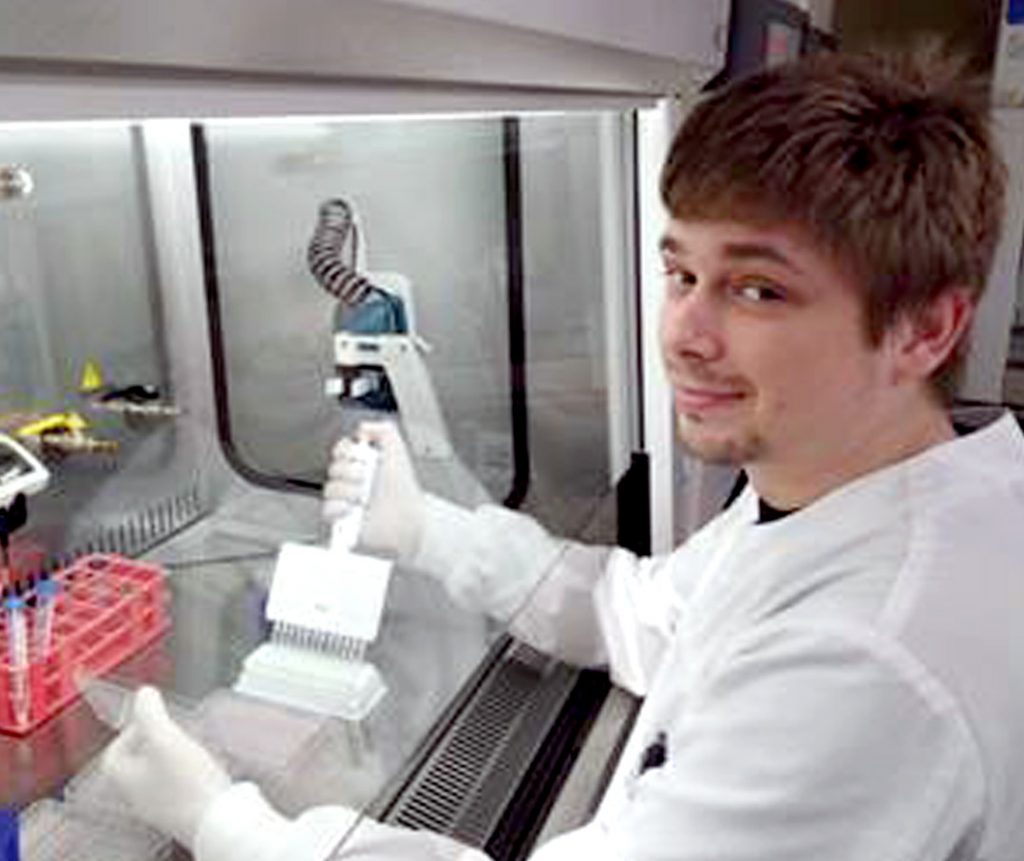
Dr Inês Pires Da Silva and Mr Jordan Conway
Research into liver metastases from cutaneous (skin) melanoma
Jordan Conway
PhD student, Uni Sydney, MIA
Immunotherapy, a form of treatment that aims to harness and boost a patients’ own immune system, is the current standard of care for patients with advanced metastatic melanoma. This treatment regimen is leading the way in increasing survival rates in patients whose melanoma has metastasised to other sites around their body. While these therapies have bettered outcomes for many patients and show promise in achieving long term control of their disease, there are still a large number of patients who do not respond to these treatments.
We are continually developing our understanding of the importance of tailored treatments that are as personalised as possible to achieve better long term outcomes for individual patients. We are now aware that the area of the body that melanoma spreads to, i.e. the liver, the lung, etc. can have a significant impact on the chances of a patient responding to therapy.
Specifically, we know patients whose melanoma has spread to their liver tend to respond worse than those without liver metastases.
The goal of my research is to understand the biological reason why our best therapies don’t work as efficiently on patients whose melanoma has spread to their liver.
My aim is to identify new immune markers within the liver that we can potentially target with new treatments in order to increase response rates. I will look within the tumour microenvironment, and assess the abundance of specific immune cells to try to identify these new targets. My goal is then to develop an experimental model that we can use in the laboratory to test on patient samples to try and identify which treatment regimen or novel treatment option may be best suited for each patient.
The development of a real-time, personalised, human model of response will enable the development of new therapy options and guide new clinical trials for patients with liver metastases, while also being utilised in routine care for all patients as a more personalised treatment approach.
September 2021 update
Jordan has the following update to share with us.
Project: liver mets from melanoma primary
The aim of our research has been to better understand the biological reasons behind why patients whose melanoma has spread to their liver are less likely to respond efficiently to our best therapy options.
To date our research has found that liver metastases are less immunogenic with fewer T cells, important for immunotherapy response, that are also further away from tumour cells compared to sites with better response to immunotherapy, such as lung metastases. We have also observed a reduced expression of PD-1 the primary target for anti-PD-1 based immunotherapy whilst observing increased expression of the immune inhibitory receptor Tim3 in liver mets compared to other sites highlighting a potential therapeutic opportunity.
We have set out to establish an experimental explant model within the lab that will allow us to test novel drugs and drug combinations on patient biopsies in an attempt to identify which treatment regime is best suited for the patients’ particular tumour. Specifically we want to use this model on patient liver biopsies to functionally test different treatment options that may lead us to drugs which confer an increased response compared to current therapy options in these patients. So far we have been able to establish a general work flow for the model that is currently still undergoing optimisation. We have also been able to run 2 pilot groups of patient samples obtained from patient tumour resections. The first group was used to establish if throughout the sample treatment it was possible to visualise immunotherapy drug infiltration through fluorescently tagged drugs whilst maintaining tumour architecture. Through this we were able to identify the areas within the tissue the drug infiltrated. Our second cohort has been used to establish the effect of an anti-PD-1 drug in this model in order to optimise timing and dosage regimes for future experiments. Work on this model is still undergoing further optimisation with Immunohistochemistry and other experiments including novel drug optimisations still to come including anti-Tim3.
Overall once this model is optimised and established in our lab we hope to be able to use this as a real-time personalised model of response for patients with metastatic disease, and more specifically in patient with liver disease to better target drug therapies to individuals based on their own tumour. This model will allow us to functionally test new and emerging drug targets under a variety of experimental conditions with the hope of eventually being able to feed this information back to the clinician to help guide treatment selection.
Research into early detection of uveal (eye) melanoma
Aaron Beasley
PhD student, Edith Cowan University, Perth
Uveal melanoma is the most common cancer of the eye in adults.
Approximately 8.6 per million per year are diagnosed with the disease in Australia. Although rare, about 50% will have spread of the disease from the eye to other organs and sites within the body, and once this occurs approximately 92% of people will die within two years. Unlike cutaneous (skin) melanoma, there are no effective systemic therapeutic agents for control of the disease. Currently, only complete surgical removal of metastatic tumour impacts overall survival. This, however, requires early detection of the disease via radiological scans, which can be unspecific and have limited sensitivity.
This project aims to develop a minimally invasive, robust and UM-specific blood test to supplement the current standard of care.
For this blood test, we will be measuring the levels of circulating tumour DNA or ctDNA present in the plasma of patients. Circulating tumour DNA is shed into the blood when cancer cells within the body die. We have previously reported that we could detect the presence of ctDNA prior to radiological scan in patients with UM, and we could even detect ctDNA in cases where the results were inconclusive.
With the wonderful support of the AMRF, we will be validating whether ctDNA can be detected before or at the time of cancer spread based on radiological scans.
At the end of the project, we will be able to show that ctDNA can enable timely detection of the cancer spread, when patients can still undergo complete tumour resection, and when available, post-operative systemic treatments for long-term survival benefit.
The outcomes of this study will provide foundational data to support a large-scale investigation on routine ctDNA testing in the management of uveal melanoma.
Mr Aaron Beasley
October 2022 update
Aaron Beasley has the following short update to share with us.
In a multicentre study (ECU, Aus; Erasmus MC, NL), we found that we could detect ctDNA in 63% of patients before (median lead time of 4.4 months) or at the diagnosis of metastatic disease. There was a positive and negative predictive value of 100% and 69%, respectively. Patients with detectable ctDNA had shorter survival, and higher levels were significantly associated with very poor outcomes. The levels of ctDNA detected were also significantly associated with disease burden measured using PET/CT, indicating ctDNAs’ use as a surrogate of total disease volume. Lastly, we monitored patients undergoing immunotherapy. We found that patients undergoing combination Ipilimumab/Nivolumab showed a one to two log reduction of ctDNA after treatment initiation, indicating some effect of the treatment on the tumour. In contrast, patients with single agent Pembrolizumab had no change in ctDNA levels.
Melanoma research
The AMRF is committed to funding research aimed at furthering knowledge and offering better outcomes in the prevention, diagnosis and treatment of melanoma.
The AMRF will focus on supporting early career researchers in Australia.
